The Ultimate Guide To Measuring And Managing Addiction Severity
Addiction is a complex and multifaceted issue that affects individuals and communities worldwide. It is a chronic condition characterized by compulsive drug seeking and use, despite harmful consequences. Measuring and managing addiction severity is crucial for effective treatment and recovery. This ultimate guide aims to provide an in-depth understanding of the assessment and management strategies for addiction, offering valuable insights for healthcare professionals, researchers, and individuals seeking support.
Understanding Addiction Severity

Addiction severity encompasses the various dimensions and impacts of substance use disorders. It goes beyond the mere presence of addiction, considering the extent and complexity of the problem. By evaluating the severity of addiction, healthcare providers can tailor treatment plans, predict outcomes, and allocate resources more efficiently.
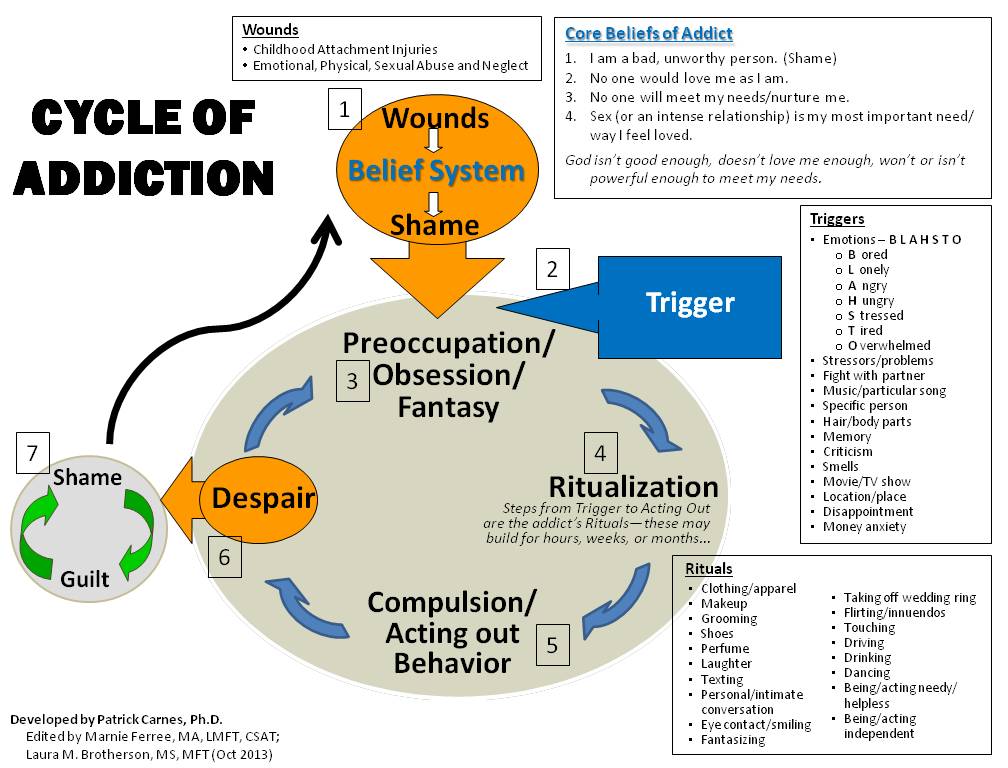
Several factors contribute to the severity of addiction, including the type and amount of substance used, the duration of addiction, co-occurring mental health disorders, social and environmental factors, and the individual's response to treatment. Understanding these factors is essential for developing a comprehensive assessment and management approach.
Assessing Addiction Severity: Tools and Techniques
Accurate assessment of addiction severity is the foundation of effective treatment. Healthcare professionals employ a range of tools and techniques to evaluate the severity and complexity of an individual’s addiction.
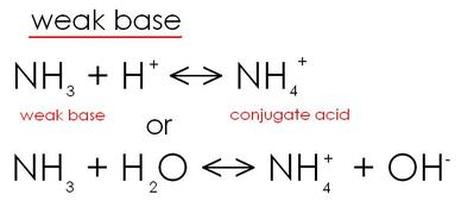
Structured Clinical Interviews
Structured clinical interviews are a standardized method used to gather detailed information about an individual’s substance use history, mental health status, and social functioning. These interviews follow a structured format, ensuring consistency and reliability in data collection. The Addiction Severity Index (ASI) is a widely used tool that assesses various domains, including medical status, employment, and family/social relationships.
Self-Report Questionnaires
Self-report questionnaires are valuable tools for assessing addiction severity. These questionnaires, such as the Alcohol Use Disorders Identification Test (AUDIT) and the Drug Abuse Screening Test (DAST), are designed to be completed by individuals themselves. They provide insights into the frequency, quantity, and consequences of substance use, allowing healthcare professionals to gauge the severity of the addiction.
Biomarkers and Laboratory Tests
Biomarkers and laboratory tests play a crucial role in assessing addiction severity. These tests can detect the presence of substances in the body, indicating recent or ongoing use. Additionally, they can provide information about the individual’s physical health, organ function, and potential complications associated with substance use. Common biomarkers include liver function tests, complete blood count, and urine drug screens.
Psychological Assessments
Psychological assessments are essential for understanding the mental health aspects of addiction severity. These assessments evaluate mood disorders, anxiety, post-traumatic stress disorder (PTSD), and other co-occurring conditions. By identifying these factors, healthcare professionals can develop integrated treatment plans that address both the addiction and the underlying psychological issues.
The Multidimensional Nature of Addiction Severity
Addiction severity is not solely determined by the amount or frequency of substance use. It is a multidimensional concept that encompasses various aspects of an individual’s life. Understanding these dimensions is crucial for a holistic approach to treatment and recovery.
Physical Health
Substance use disorders can have severe physical health consequences. Chronic substance abuse can lead to organ damage, cardiovascular issues, respiratory problems, and an increased risk of infectious diseases. Assessing and managing physical health is vital for the overall well-being of individuals with addiction.
Mental Health
Co-occurring mental health disorders are common among individuals with addiction. Depression, anxiety, bipolar disorder, and personality disorders can contribute to the severity of addiction and complicate treatment. Integrated treatment approaches that address both addiction and mental health are essential for successful recovery.
Social and Environmental Factors
The social and environmental context in which an individual lives can significantly impact addiction severity. Factors such as family dynamics, peer influence, socioeconomic status, and access to resources can either support or hinder recovery. Social support networks, stable housing, and community-based interventions are crucial components of effective addiction management.
Treatment Planning and Intervention Strategies
Once addiction severity has been assessed, the next step is to develop a comprehensive treatment plan. Treatment planning involves considering the individual’s unique needs, preferences, and goals, as well as the severity and complexity of their addiction. Evidence-based interventions and tailored strategies are employed to address the various dimensions of addiction severity.
Pharmacological Interventions
Pharmacological interventions play a crucial role in managing addiction severity. Medications can help reduce cravings, manage withdrawal symptoms, and prevent relapse. For example, methadone and buprenorphine are commonly used in the treatment of opioid use disorders, while disulfiram and naltrexone are effective for alcohol use disorders. The choice of medication depends on the specific substance involved and the individual’s response.
Behavioral Therapies
Behavioral therapies are essential components of addiction treatment. These therapies aim to modify thoughts, emotions, and behaviors related to substance use. Cognitive-behavioral therapy (CBT), motivational interviewing, and contingency management are evidence-based approaches that have shown effectiveness in reducing addiction severity and promoting long-term recovery.
Supportive Interventions
Supportive interventions provide individuals with addiction the necessary tools and resources to manage their recovery. These interventions include peer support groups, such as Alcoholics Anonymous (AA) and Narcotics Anonymous (NA), which offer a sense of community and mutual support. Additionally, family therapy and counseling can help improve family dynamics and address interpersonal issues that may contribute to addiction severity.
Measuring Treatment Outcomes and Success

Measuring the outcomes and success of addiction treatment is crucial for evaluating the effectiveness of interventions and making informed decisions. Various tools and metrics are used to assess treatment progress and determine the severity of addiction over time.
Clinical Outcomes
Clinical outcomes measure the reduction in addiction severity and the improvement in overall well-being. These outcomes include reduced substance use, improved physical and mental health, and increased social functioning. Regular assessments and follow-up evaluations help track progress and identify areas that may require further intervention.
Biomarker Analysis
Biomarker analysis is a valuable tool for monitoring treatment outcomes. By analyzing biological markers, healthcare professionals can assess the effectiveness of interventions and detect any potential relapses. For example, urine drug screens can indicate ongoing substance use, while liver function tests can reflect improvements in organ health.
Patient-Reported Outcomes
Patient-reported outcomes provide valuable insights into the individual’s perception of their recovery journey. These outcomes include measures of quality of life, satisfaction with treatment, and self-reported changes in substance use. Patient-reported outcomes complement clinical and biomarker assessments, offering a holistic view of treatment success.
Addressing Barriers and Challenges in Addiction Management
Managing addiction severity comes with its own set of challenges and barriers. Healthcare professionals must navigate these obstacles to ensure effective treatment and support for individuals with addiction.
Stigma and Discrimination
Stigma and discrimination are significant barriers to addiction management. Negative attitudes and stereotypes surrounding addiction can deter individuals from seeking help and accessing treatment. Healthcare professionals play a crucial role in combating stigma by providing education, promoting empathy, and advocating for equal access to healthcare services.
Access to Treatment
Limited access to treatment is a common challenge in addiction management. Barriers such as financial constraints, lack of transportation, and long wait times can prevent individuals from receiving timely and appropriate care. Addressing these barriers requires collaborative efforts between healthcare providers, policymakers, and community organizations to improve access and reduce treatment disparities.
Relapse and Recurrence
Relapse is a common occurrence in addiction recovery. It is essential to recognize that relapse does not indicate treatment failure but rather a natural part of the recovery process. Healthcare professionals should focus on relapse prevention strategies, such as developing coping skills, addressing triggers, and providing ongoing support and monitoring.
The Role of Technology in Addiction Management
Technology has revolutionized the field of addiction management, offering innovative tools and resources to support individuals in their recovery journey.
Digital Therapeutic Platforms
Digital therapeutic platforms provide accessible and convenient tools for addiction management. These platforms offer a range of features, including educational content, self-assessment tools, and interactive therapy modules. By leveraging technology, individuals can access evidence-based interventions and support whenever and wherever they need it.
Telehealth and Remote Monitoring
Telehealth and remote monitoring have become increasingly important in addiction management, especially in the context of limited in-person interactions. These technologies enable healthcare professionals to provide remote assessments, counseling, and medication management. Remote monitoring systems can also track vital signs, substance use patterns, and treatment adherence, allowing for early intervention and timely support.
Mobile Applications
Mobile applications have emerged as powerful tools for addiction management. These apps offer a range of features, such as relapse prevention strategies, mood tracking, and peer support. By leveraging the ubiquity of smartphones, individuals can access personalized support and resources, empowering them to take an active role in their recovery.
The Future of Addiction Severity Management
The field of addiction severity management is continuously evolving, driven by advancements in research, technology, and clinical practice. As our understanding of addiction deepens, new approaches and interventions are being developed to enhance treatment outcomes and support long-term recovery.
Personalized Medicine
Personalized medicine is an emerging approach that tailors treatment plans to an individual’s unique genetic, environmental, and behavioral factors. By considering these factors, healthcare professionals can develop more effective and targeted interventions. Genetic testing, for example, can identify specific genetic variations that influence an individual’s response to certain medications, allowing for more precise treatment decisions.
Integrative and Complementary Therapies
Integrative and complementary therapies are gaining recognition as valuable additions to traditional addiction treatment. These therapies, such as mindfulness-based interventions, yoga, and acupuncture, focus on the mind-body connection and holistic well-being. By incorporating these approaches into treatment plans, individuals can explore alternative strategies for managing addiction severity and promoting overall health.
Data-Driven Approaches
Data-driven approaches are revolutionizing addiction management by leveraging large-scale data and advanced analytics. By analyzing vast amounts of data, healthcare professionals can identify patterns, predict outcomes, and develop more effective treatment strategies. Machine learning algorithms, for instance, can analyze patient data to identify risk factors and personalize treatment plans based on individual characteristics.
Conclusion
Measuring and managing addiction severity is a complex and multifaceted process that requires a comprehensive understanding of the individual’s unique needs and circumstances. By employing a range of assessment tools, evidence-based interventions, and supportive strategies, healthcare professionals can effectively address the multidimensional nature of addiction severity. As the field continues to evolve, the integration of technology, personalized medicine, and data-driven approaches holds great promise for improving treatment outcomes and supporting individuals on their journey to recovery.
How long does it take to recover from addiction severity?
+The recovery process from addiction severity varies from person to person. It depends on several factors, including the individual’s commitment to treatment, the severity of their addiction, and the presence of co-occurring disorders. On average, it can take several months to a few years to achieve long-term recovery. However, it is important to note that recovery is an ongoing journey, and individuals may experience setbacks and relapses along the way. Continuous support, relapse prevention strategies, and ongoing monitoring are crucial for maintaining progress and achieving sustained recovery.
Can addiction severity be cured completely?
+Addiction is considered a chronic condition, and there is no definitive cure. However, with proper treatment and ongoing support, individuals can achieve long-term recovery and manage their addiction effectively. It is important to view addiction as a manageable disease, similar to other chronic conditions such as diabetes or hypertension. By adopting a holistic approach that addresses the physical, mental, and social aspects of addiction, individuals can lead fulfilling lives and reduce the severity of their addiction over time.
What are the signs of improving addiction severity?
+Improving addiction severity is indicated by several positive changes. These include a reduction in substance use, improved physical and mental health, increased social functioning, and enhanced overall well-being. Individuals may also experience a decrease in cravings, better impulse control, and improved decision-making abilities. Additionally, positive changes in relationships, employment, and legal status can be indicators of improving addiction severity. It is important to note that progress may be gradual, and setbacks are common, but with consistent effort and support, individuals can achieve significant improvements in their addiction severity.